“Here, at a point when the will is the highest danger, art approaches, as a saving, healing magician. Art alone can turn those thoughts of disgust at the horror or absurdity of existence into imaginary constructs which permit living to continue.”
– Nietzsche, The Birth of Tragedy
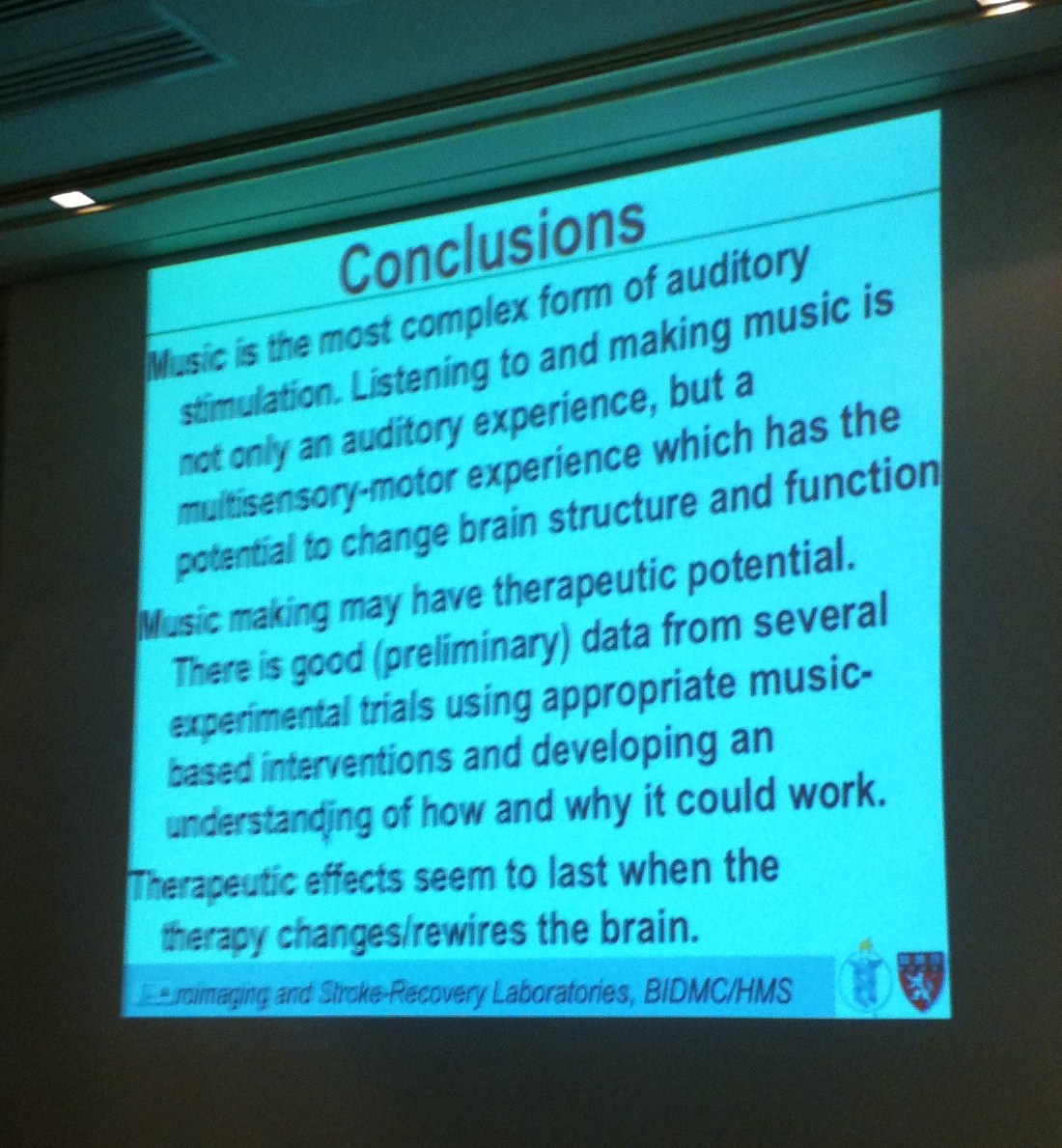
Though I’ve held an interest in music’s healing capacities for many years, it’s only recently come to my attention just how quickly the field is growing. Music therapy is a practice in which an MT (Music Therapist) uses music-based interventions to address non-music goals with a client. As music is multi-modal, engages the brain and body across multiple domains, and is adaptable for people of all abilities, it continues to show promise in the medical field. With the growing prevalence of conditions such as autism and Alzheimer’s as well as the steady improvement in diagnostic means, the demand for music therapy professionals in higher than ever.
With the many recent developments in the field of dementia research, I have often found myself in dialogue with friend and colleague James Gutierrez (Ph.D. in progress, UCSD), especially in regard to current criticism of music therapy. As we both appreciate the consequence of the more basic, affective measures of music in creative practice as it applies to the therapeutic setting while retaining a firm belief in the necessity of empirical, effect-based evidence, I’ve had the pleasure of benefitting from many edifying conversations of this nature.
In music therapy, a common issue arises from the type manner research is conducted within the field, which is often achieved in the form of anecdotes, observations, and more qualitative data. As this is the case, many professionals and scholars in the field of medicine tend to “write off” such evidence as circumstantial and struggle to find the distinction between music therapy and “music as therapy.”
In the recent paper, Music Therapy in the Care of Cognitive Decline: Between affective and effective treatment (2014) Gutierrez does an excellent job of addressing many of these current issues, choosing to focus most intently on the application of music therapy in patients suffering from dementia. Coming from a place of unique understanding, he combines solid, objective exploration in conjunction with more personal, poignant observations into concepts of identity, agency, and consciousness seldom found in an often dispassionate world of research. The following edit consists of excerpts I have found to be of particular interest to the layman and scientist alike. The paper may be read in its entirety here.
Medical science in the modern age has, in the spirit of modernism, delighted in expunging any and all traces of the magical and mystical from the proper, scientific treatment of the human body. Even while archeological evidence suggests music’s wide centrality to medicinal healing practices for untold eras of human history[1], the Cartesian dualism that yet pillars modern medicine provides reason to station music as a matterless matter of the mind, with medical practice operates as the material treatment of the body. For inasmuch as medical science is a category whose domain includes anatomical structures and physiological processes, only health practices subject to empirical testing, measurement, observation, and quantification are considered proper ‘medication’. However, as the research of recent years has begun to unearth the complex physiological effects (not just affects) of music listening and musical practice, the critical gaze of medical science is beginning to shift, poised to reasonably reevaluate the efficacy of this timeless healing magician not just of the mind, but also of the brain and body.
The American Music Therapy Association defines Music Therapy as “the clinical and evidence-based use of music interventions to accomplish individualized goals within a therapeutic relationship by a credentialed professional who has completed an approved music therapy program.” Outside the field of music therapy, particularly within burgeoning cognitive and neurological research, viable theories that attempt to explain the physical mechanics are gaining traction within the medical community. This research could be furthered by continuing to build upon an embodied and enactive approach to cognition, as such an ecological perspective not only shifts the aesthetic conversations away from stale romantic dualisms within artistic communities, but invites all who make the human body their subject to reconsider their most basic assumptions.
Among the most common areas of music therapy is in its implementation in the treatment (used loosely) of dementia and Alzheimer’s disease. Music therapy is not only gaining popularity among clinicians in end-of-life care for its astounding cost/benefit ratio, but is also spreading as the rising occurrences of these diseases increase demand. In anticipation of this rise several organizations have begun to push for renewed focus on prevention and treatment. On February 26th, 2014, actor/comedian Seth Rogen testified before the Senate Appropriations Subcommittee on Labor, Health, and Human Services to raise awareness about Alzheimer’s Disease and promote his research-funding charities.[2] This comes on the heels of the historic “National Plan to Address Alzheimer’s Disease” released by the U.S. Department of Health and Human Services in May 2012, calling for preventing and effectively treating Alzheimer’s disease by 2025.
This central focus has been brought to my attention through my own grandmother’s rapidly declining cognitive state and subsequent placement in the care of a hospice facility. To witness a loved one’s gradual decline into self-obscurity through loss of memory and awareness is not only tragic, as anyone who has done so will agree, but also perplexing, precisely because it challenges our conception of identity, not only theirs but ours as well. Once, after a particularly discouraging visit with my grandmother, when for the first time it took a matter of minutes for her to recognize her own daughter, my mother confessed “she is no longer my mother; not the mother that I know.” Any theory of consciousness desiring to describe the nature of the human state of mind when at its most ‘stable’ must also be tested to account for consciousness when at its most volatile- when autonoesis fails and all is a static cloud, when active agency slowly melts into a passive patiency, when all psychosocial capacities disintegrate involuntarily and nothing remains but inert solipsism. It is through studying this transitory final act when inner lights begin to dim and everything becomes strange and unfamiliar, that we can truly test what is meant by consciousness, and where all notions of mind and body essentially converge. Since music research from virtually all angles repeatedly reveal how immensely deep it delves into our individual identity and how expansively broad it affords a robust social identity, it is only too obvious for music to be deployed in the intervention of a fading consciousness.
Much has been written about music therapy as a tool to improve quality of life, if not also to slow the symptoms of dementia in the best scenarios, with most reports centering on qualitative research and anecdotal accounts. This softer focus on success stories may be par for the course, after all, end-of-life research is a tender field, and family members and medical staff typically have much more on their mind than entertaining the abstract probing of a curious consciousness theorist. Thus, for better or for worse, many of the most salient questions are left unasked.
Music as Therapy
At this point it is important to review the recent literature concerning the implementation of music in the treatment of dementia and Alzheimer’s Disease (AD). The slow march towards a pharmaceutical cure feels optimistic, but does not seem promising. Moreover the monetary cost and side effects from the drugs currently available upset the cost/benefit ratio when considering the overall quality of life for an individual in palliative and hospice care. These factors have contributed to the growth of stimulatory therapies, including music therapy, in its appeal to virtually all involved (except, presumably, the pharmaceutical corporations). Music therapy, specifically, has grown more than any other due to its incredible cost/benefit ratio. The more we learn about neuroplasticity, and the deeply embodied/embedded/enactive nature of music cognition, the stronger the case become for music as a viable therapeutic treatment.[3]
Perhaps the most promising neurological support to the claims and efforts of music therapy hinge on the emerging studies within the mirror neuron system [MNS]. Though not much can be said for certain about these structures, particularly as they relate to humans, their ‘discovery’ has nonetheless provided an exciting new platform for discussing virtually any field of human interaction and learning, encouraging interdisciplinary discussions, and fostering theoretical models that render a classical cognitive model increasingly problematic through emphasizing inter/intra connectivity, and shared cognition.[4]
Building on MNS theories, one recent model offers a strong base toward a more substantive base for music therapy is the Shared Affective Motion Experience (SAME) model, which suggests that musical sound is perceived not only in terms of the auditory signal, but also in terms of the intentional, hierarchically organized sequences of expressive motor acts behind the signal. Thus, the expressive dynamics of heard sound gestures may be interpreted in terms of the expressive dynamics of personal vocal and physical gestures.
According to SAME, in observing the actions of others our MNS continuously compares predicted motions (kinematics) with observed motions in attempt to minimize the prediction error, enabling the observer to determine the most likely cause of the action at all levels: intention, goal, motor, and kinematic. This pull toward minimized prediction error would explain the effectiveness of personalized iPods over live musical interaction on reducing anxiety for dementia/AD patients. In addition to providing a harder base for the previously cited Psychosocial Model of music therapy, the SAME model also correlates to theories of embodied mind and intersubjective consciousness.
To regard the practice of music therapy as a psychotherapeutic stimulation therapy, and a marginal one at that, is understandable from a classical cognitivist perspective in which music exists representationally as auditory percepts to be processed with limited physiological impact. This is perhaps why present discussions regard music therapy as limited to its affective capacities in emotional support, palliative quality of life, and feelings of happiness; categorically separate from pharmaceutical medications which are understood to truly effect ones physiology. However, in positing a more deeply embodied perspective of music as a perturbation/compensation in a richly physical dynamic interaction between bodily experience and neural processes, there emerges a view of cognition that troubles the affect/effect dichotomy, and with it, assumptions of what criterion constitute legitimate vs. illegitimate medical treatments.
Music as therapy has its limitations, to be sure, and music therapy stands to discredit its case by overstating what relatively little research has yet been able to substantiate its claimed miracles. Becoming ever clearer, however, is that its limitations are not well described by the standard cognitivist model that dominates medical and psychological sciences. As embodied cognition grows in establishment, the doors widen for music therapy, and other traditionally holistic care practices, to further state, test, and prove their case as a valid treatment in the care of the human mind, particularly an embodied mind.
[1] Conrad, Claudius, Music for healing: from magic to medicine, The Lancet, Volume 376, Issue 9757, pg. 1980, Dec. 2010
[2] Seth Rogen Opening Statement (C-SPAN), Feb. 26th, 2014 http://www.youtube.com/watch?v=UHqx3-mfHAY
[3] N. Simmons-Stern, R. Deason, B. Brandler, B. Frustace, M. O’Conner, B. Ally, and A. Budson, Music-Based Memory Enhancement in Alzheimer’s Disease: Promise and Limitations, Neuropsychologia. 2012 December ; 50(14): 3295–3303
[4] There is some debate whether or not mirror neurons support classical representationalism



 Susann Siggel1,
Susann Siggel1, 



You must be logged in to post a comment.